The Benefits Suite in Interact SSAS is a powerful, integrated set of modules designed to manage the entire lifecycle of benefit claim processing within a Social Security Administration. From the submission of medical certificates and claims to multi-tiered approvals, third-party payments, and the final generation of award letters, each component ensures that beneficiaries receive accurate, timely, and compliant benefit services.
Built on highly configurable workflows and integrated medical and financial systems, this suite enables transparent processing, auditability, and seamless service delivery to individuals and institutions alike. Whether managing a sickness claim, processing refunds to employers, or producing official correspondence, the suite supports each stage with security, efficiency, and flexibility.
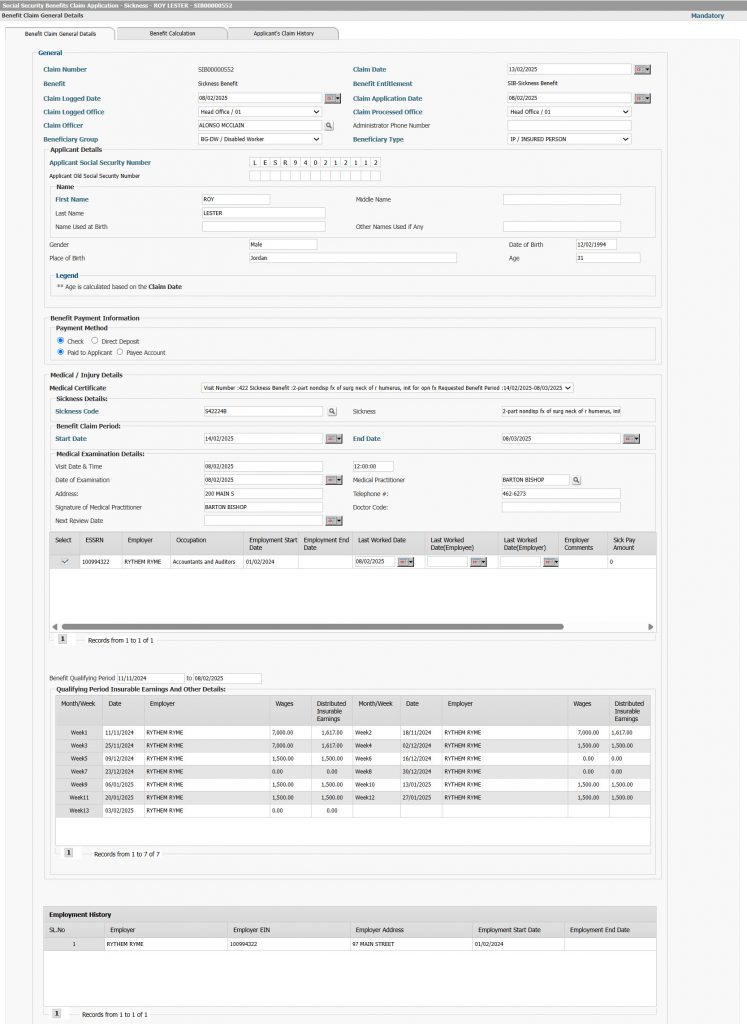
Benefit Claims Filing Management
Figure 1: Benefit claim
Purpose: Manages the complete benefit claim lifecycle, including submission, review, employer verification, SSA approval, and readiness for payment.
- Unlimited benefit classes and entitlement rules
- Online e-Services claims with pre-filled claimant/employer data
- Employer sick pay validation and work history checks
- SSA claim audit, medical review, and payment approval
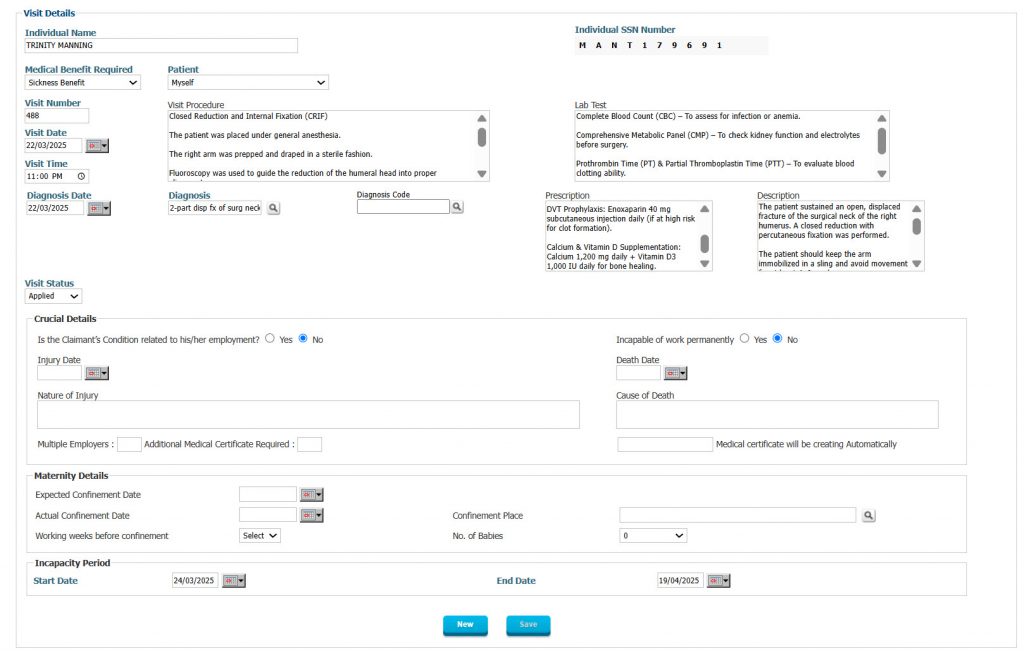
Medical Visits and Diagnosis Management
Figure 2: Medical certificate with diagnosis
Purpose: Tracks and manages all medical information used to assess benefit eligibility for sickness, maternity, disability, and invalidity benefits.
- Direct entry of medical records by healthcare providers
- Medical certificate generation and electronic submission
- SSA review of diagnosis, incapacity, and recommended benefits
- Optional review by medical referees for high-stakes cases
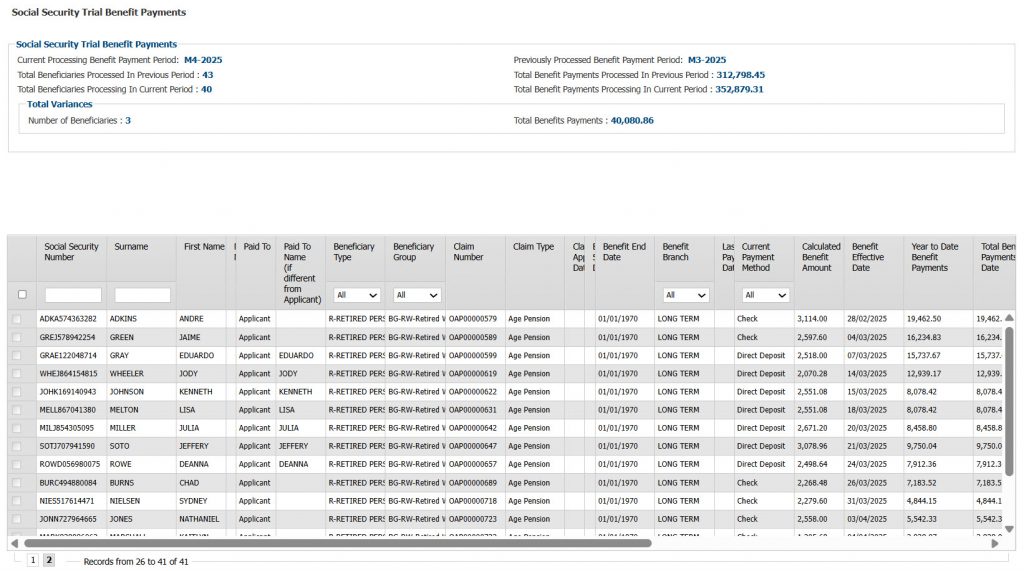
Benefit Claims Payment Management
Figure 3: Benefit claims trial process
Purpose: Oversees the full cycle of benefit payment processing, from trial validation to final disbursement and reconciliation.
- Payment cycle initialization based on custom calendars
- Trial ACH, check, and GL posting validation
- Final disbursement with secure approval and audit trail
- Handles suspended claims and period closing
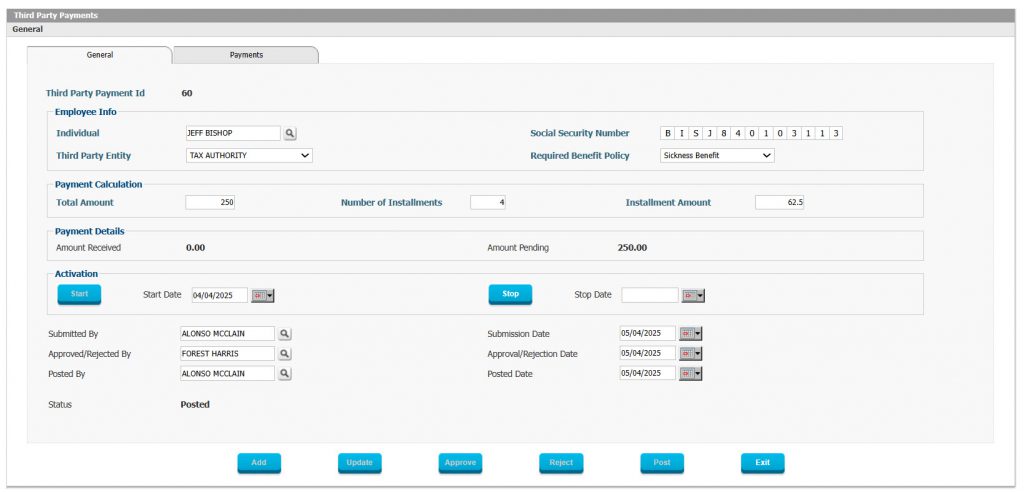
Third-Party Payments
Figure 4: Third-party payment
Purpose: Allows social security administrations to pay third-party entities on behalf of beneficiaries for legal, healthcare, or institutional obligations.
- Supports healthcare, court, and tax-related payments
- Authorization linked to claims or legal mandates
- Secure processing and tracking of disbursements
- Prevents duplicate or unauthorized payments
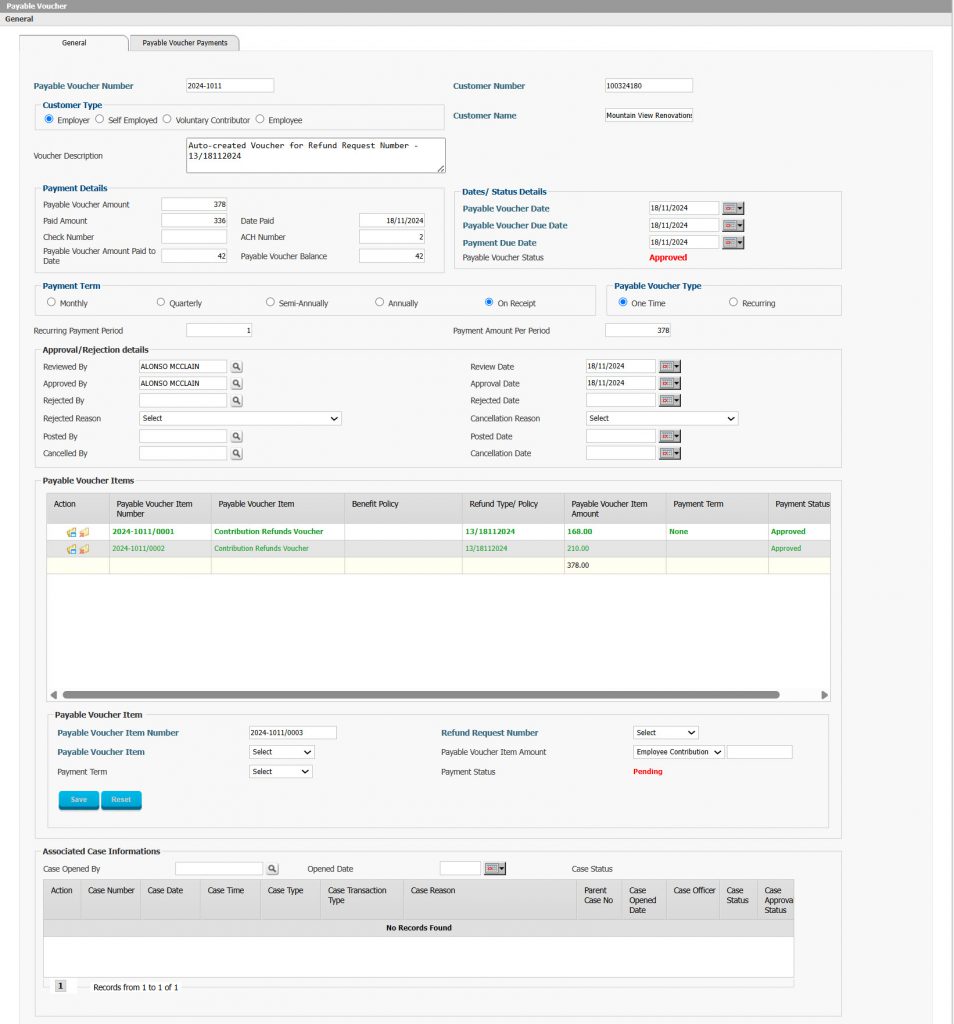
Payables Management
Figure 5: Payables voucher
Purpose: Adds an optional internal control layer through Payable Vouchers before funds are disbursed for claims or refunds.
- Voucher generation upon claim/refund approval
- Manual review, update, or rejection of vouchers
- Final payment only permitted after voucher approval
- Full integration with GL, e-Services, and refund modules
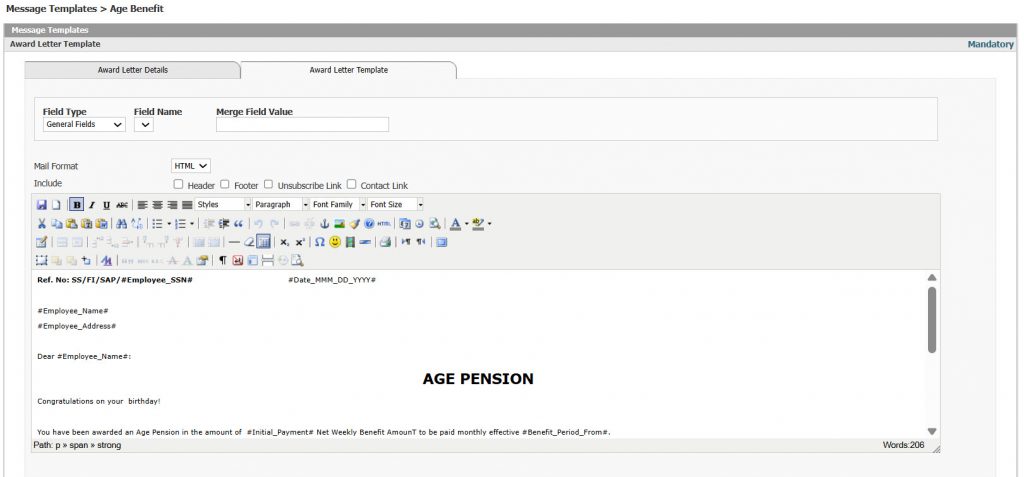
Award Letters Management
Figure 6: Award letters template creation
Purpose: Automates the generation of official benefit letters to notify beneficiaries of approvals, rejections, or audit outcomes.
- Customizable templates with dynamic data fields
- Letters stored in beneficiary profile and e-Services
- Workflow-driven generation based on claim events
- Integrated with Compliance and Document Management